Before we talk about the current state of affairs of the “physician’s mind”, let me emphasize the following quote:
“Go beyond your mind change your attitude…your perspective… your angle, your mode of vision. The new state of affairs has arrived, but you are not going to see it unless you change”. Fr. Robert Barron.
There is ample evidence to support the pandemic of burnout among physicians, nurses, and healthcare executives. With rates across all specialties averaging around 50 %, the consensus is that it is way overdue to develop concrete applicable solutions to help mitigate the impact of burnout, protect against it, and help professionals change from a state of being reactive to a state of being proactive state.
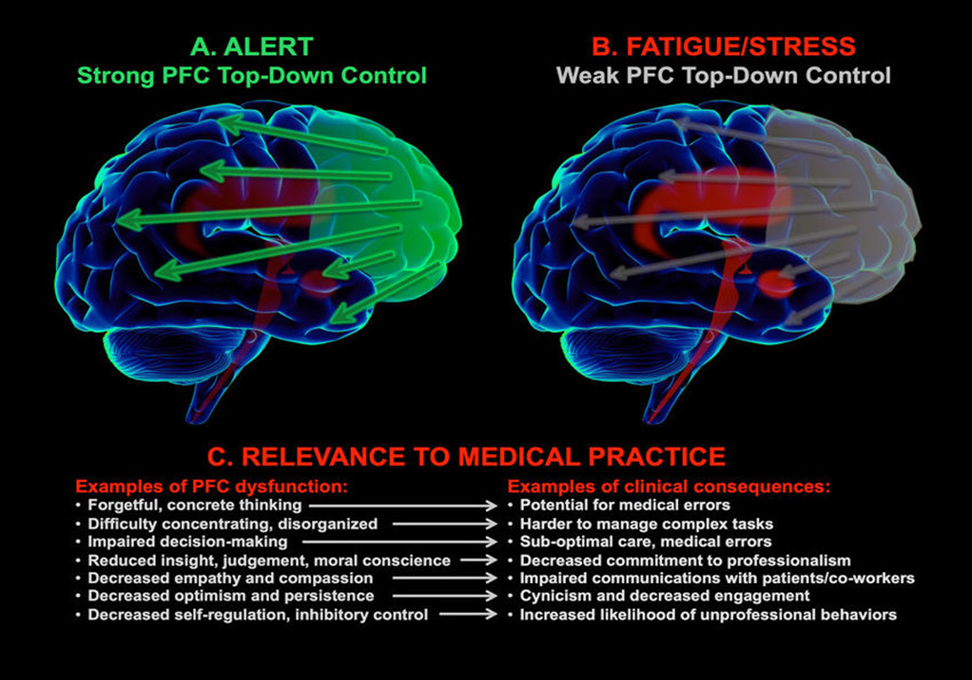
The focus of the new state of affairs is the pre-frontal cortex. This is where the majority of the pathology and organic changes occur. Since we are discussing organic disease, let us discuss pathophysiology and contributing factors. And if we are to summarize those factors into one word, let us choose: STRESS!
Some definitions:
Stress is the feeling of being overwhelmed or unable to cope with mental or emotional pressure.
Stress is the internal resistance, or counterforce, of a material to the distorting effects of an external force or load.
Let us expand a little bit. There are EXTERNAL and INTERNAL distorting forces at work here that STRESS our minds. That necessitates a response. That response can sometimes be beneficial. However, in the case of burnout and our current state of affairs, the response mostly the exact opposite.
According to the WHO, burnout is a “Syndrome conceptualized as resulting from chronic workplace stress that has not been successfully managed.” Burnout is an occupational phenomenon. When we are removed from the stressful environment, our brains usually recover. However, the impact of stress does not stop at burnout. Sadly, some changes are much more profound and much more permanent.
A timeline of mental changes (Kirch, 2021)
:
- Medical students: At entry point, mental health is similar to the rest of the population.
- Medical students year 2: 57 % had moderate to severe symptoms of anxiety, 27 % had symptoms of depression.
- Medical students’ mental health significantly declines after end of year 2
- At the end of medical school, 22 % of those depressed and 42 % of those suicidal utilize mental health support. The rest DO NOT!
- During residency and afterwards, women had a higher prevalence of mental disorders than men (24.5 % vs 16.3 %)
- Prevalence rate per age group: Age group 18-25: 29.4 %. Age group 26-49: 25%. Above 50: 14.1 %.
- 66 % of male and 58% of female MDs with burnout had never received professional help and do not plan to seek it!
A closer look at the effects of stress on the prefrontal cortex reveals the following (Haines & Arnsten, 2008; McEwen, Gray, and Nasca, 2015):
- The pathogenesis of psychiatric diseases including depression and anxiety disorders involves dysregulated prefrontal control over amygdala
- Among the environmental factor most linked to such mental illnesses is stress
- Chronic stress leads to worsening of these effects that can last even after stress is removed
- With chronic stress, there are additional architectural changes that further exaggerate the switch from highly evolved to more primitive brain circuits
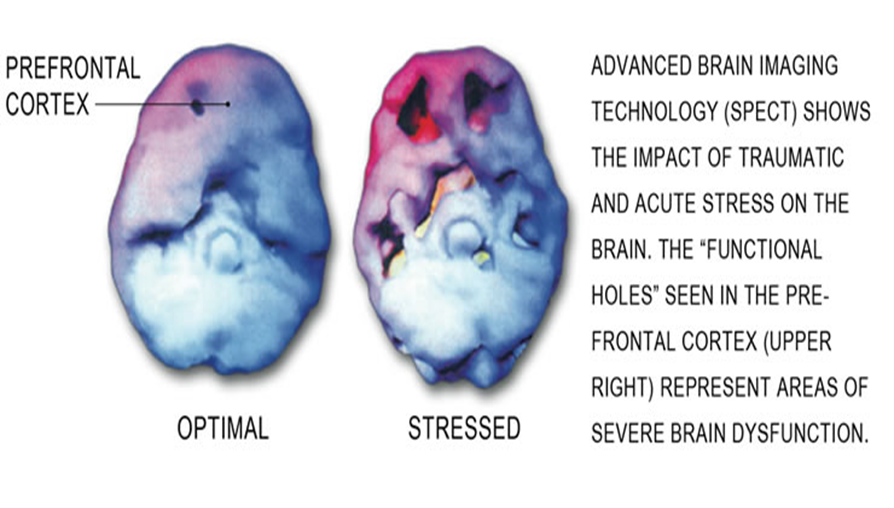
A closer look at what happens on the organic level shows the following images and effects (Davis et al, 2017):
Some of that translates into the following data and statistics:
Increase in PTSD, anxiety, depression, burnout, moral illness, and even bipolar disorders (Walton, Murray, and Christian, 2020).
From The Physicians Foundation 2020 Physician Survey: Part 2
-18 percent of physicians have increased their use of medications, alcohol, or illicit drugs
-By contrast, 13 percent of physicians have sought medical attention for a mental health problem
-50 percent of physicians have experienced inappropriate anger, tearfulness, or anxiety
-30 percent of physicians feel hopeless or that they have no purpose
-58 percent of physicians often have feelings of burnout, compared to 40 percent in 2018
“The simple reality is that becoming a physician in no way removes one’s shared human vulnerability to mental disorders.” Darrell Kirch, MD
Where can we start and what can we do?
“Before you heal someone, ask him if he is willing to give up the things that made him sick.” Hippocrates.
The process of healing starts with you. But before you can heal, ask yourself if you are willing to change some of the things that got you here! This is ORGANIC brain disease we are dealing with. So, do you believe we REALLY HAVE A CHOICE?
I have stated that stress is because of internal and external factors. While we tackle both, it’s a good place to start within. The change will occur faster, more decisively, and it is more within our control. Control it turns out, is of significant importance for physicians (Shapiro et al, 2011).
“Psychological research has demonstrated that the desire for a “sense of control,” which we define as “the ability (or perception that one has the ability) to cause an effect in the intended direction” is a pervasive human experience.” Loss of control for physicians comes from:
- Disease progression
- Patient compliance
- Regulatory requirements
- Healthcare industry demands
- “ …a healthy sense of control should include not only ways to exercise positive mastery, but also constructive acceptance of lack of control”.
It is not the intention of this blog to discuss the approaches towards combating burnout and mental health disorders. Rather, it is to bring to light the darkness that is happening in our brains. It is a CALL TO ACTION.
The consequences are real and serious. A new Survey Reveals 55% of Physicians Know a Physician Who Considered, Attempted or Died by Suicide…The Physician foundation August 2021 Survey
I am asking, no pleading, of you to be honest with yourself. If you have symptoms of burnout and the other stated mental disorders, please seek help. And if you see it in others, please seek to help them. The projections are that the organic changes in our brain are going to get worse. As the COVID pandemic starts to wind down, we expect more PTSD and other diseases to show. During a war, soldiers do not suffer from PTSD usually. It is mostly after that that this occurs.
“Diagnose the past, declare the present, foretell the future.” Hippocrates.
We share a unique past, a common present, and an individual future. It is way past the time to take the present seriously, and ensure a brighter and healthier future.
References:
- Davis MT, Holmes SE, Pietrzak RH, Esterlis I. Neurobiology of Chronic Stress-Related Psychiatric Disorders: Evidence from Molecular Imaging Studies. Chronic Stress (Thousand Oaks). 2017;1:2470547017710916. doi:10.1177/2470547017710916
- Hains AB, Arnsten AF. Molecular mechanisms of stress-induced prefrontal cortical impairment: implications for mental illness. Learn Mem. 2008 Aug 6;15(8):551-64. doi: 10.1101/lm.921708. PMID: 18685145.
- Kirch, Darrell G. MD Physician Mental Health: My Personal Journey and Professional Plea, Academic Medicine: May 2021 – Volume 96 – Issue 5 – p 618-620 doi: 10.1097/ACM.0000000000003942
- McEwen BS, Gray J, Nasca C. Recognizing Resilience: Learning from the Effects of Stress on the Brain. Neurobiol Stress. 2015;1:1-11. doi:10.1016/j.ynstr.2014.09.001
- Shapiro J, Astin J, Shapiro SL, Robitshek D, Shapiro DH. Coping with loss of control in the practice of medicine. Fam Syst Health. 2011 Mar;29(1):15-28. doi: 10.1037/a0022921. PMID: 21417521.
- Walton M, Murray E, Christian MD. Mental health care for medical staff and affiliated healthcare workers during the COVID-19 pandemic. Eur Heart J Acute Cardiovasc Care. 2020;9(3):241-247. doi:10.1177/2048872620922795